Printable Braden Scale
3A: Pressure Ulcer Prevention Pathway for Acute Care
The Braden Scale is a scale made up of six subscales, which measure elements of risk that contribute to either higher intensity and duration of pressure, or lower tissue tolerance for pressure. These are: sensory perception, moisture, activity, mobility, friction, and shear. BRADEN SCALE – For Predicting Pressure Sore Risk Use the form only for the approved purpose. Any use of the form in publications (other than internal policy manuals and training material) or for profit-making ventures requires additional permission and/or negotiation. Braden Scale Activity Categories. The Braden Scale activity categories are broken down by: Bedfast: confined to bed—think of residents with severe stroke, spinal cord injury, on bedrest due because of a wound or other issue. Chairfast: ability to walk severely limited or nonexistent. These persons cannot bear own weight and/or must be.
Background: This tool is an example of a clinical pathway, detailing the relationship among the different components of pressure ulcer prevention.
Reference: Developed by Zulkowski and Ayello (2009) in conjunction with the New Jersey Hospital Association Pressure Ulcer Collaborative.
Use: This tool can be used by the hospital unit team in designing a new system, as a training tool for frontline staff, and as an ongoing clinical reference tool on the units. This tool can be modified or a new one created to meet the needs of your particular setting. If you prepared a process map describing your current practices, you can compare that to desired practices outlined on the clinical pathway.
Pressure Ulcer Prevention Pathway
3B: Elements of a Comprehensive Skin Assessment
Background: This sheet summarizes the elements of a correct comprehensive skin assessment. You could, for example, integrate them into your documentation system or use this sheet for staff training.
Reference: Developed by Boston University Research Team.
Skin Temperature
- Most clinicians use the back rather than the palm of their hand to assess the temperature of a patient's skin.
- Remember that increased skin temperature can be a sign of fever or impending skin problems such as a Stage I pressure ulcer or a diabetic foot about to ulcerate.
- Touch the skin to evaluate if it is warm or cool.
- Compare symmetrical body parts for differences in skin temperature.
Printable Braden Scale Pdf
Skin Color
- Ensure that there is adequate light.
- Use an additional light source such as a penlight to illuminate hard to see skin areas such as the heels or sacrum.
- Know the person's normal skin tone so that you can evaluate changes.
- Look for differences in color between comparable body parts, such as left and right leg.
- Depress any discolored areas to see if they are blanchable or nonblanchable.
- Look for redness or darker skin tone, which indicate infection or increased pressure.
- Look for paleness, flushing, or cyanosis.
- Remember that changes in coloration may be particularly difficult to see in darkly pigmented skin.
Skin Moisture
- Touch the skin to see if the skin is wet or dry, or has the right balance of moisture.
- Remember that dry skin, or xerosis, may also appear scaly or lighter in color.
- Check if the skin is oily.
- Note that macerated skin from too much moisture may also appear lighter or feel soft or boggy.
- Also look for water droplets on the skin. Is the skin clammy?
- Determine whether these changes localized or generalized.
Skin Turgor
- To assess skin turgor, take your fingers and 'pinch' the skin near the clavicle or the forearm so that the skin lifts up from the underlying structure. Then let the skin go.
- If the skin quickly returns to place, this is a normal skin turgor finding.
- If the skin does not return to place, but stays up, this is called 'tenting,' and is an abnormal skin turgor finding.
- Poor skin turgor is sometimes found in persons who are older, dehydrated, or edematous, or have connective tissue disease.
Skin Integrity
- Look to see if the skin is intact without any cracks or openings.
- Determine whether the skin is thick or thin.
- Identify signs of pruritis, such as excoriations from scratching.
- Determine whether any lesions are raised or flat.
- Identify whether the skin is bruised.
- Note any disruptions in the skin.
- If a skin disruption is found, the type of skin injury will need to be identified. Since there are many different etiologies of skin wounds and ulcers, differential diagnosis of the skin problem will need to be determined. For example is it a skin tear, a pressure ulcer, or moisture-associated skin damage or injury?
3C: Pressure Ulcer Identification Notepad
Background: Reporting of abnormal skin findings among nursing staff is critical for pressure ulcer prevention. This notepad can be used by nursing aides to report any areas of skin concern to nurses.
Reference: This material originated from Status Health and was adapted for use by Mountain-Pacific Quality Health, the Medicare quality improvement organization for Montana, Wyoming, Hawaii, and Alaska, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. Contents presented do not necessarily reflect CMS policy. The work was performed under the 9th Statement of Work, MPQHF-AS-PS-09-16.
Instructions: Place an X on any suspicious lesion and give the note to a nurse for followup on the issue.
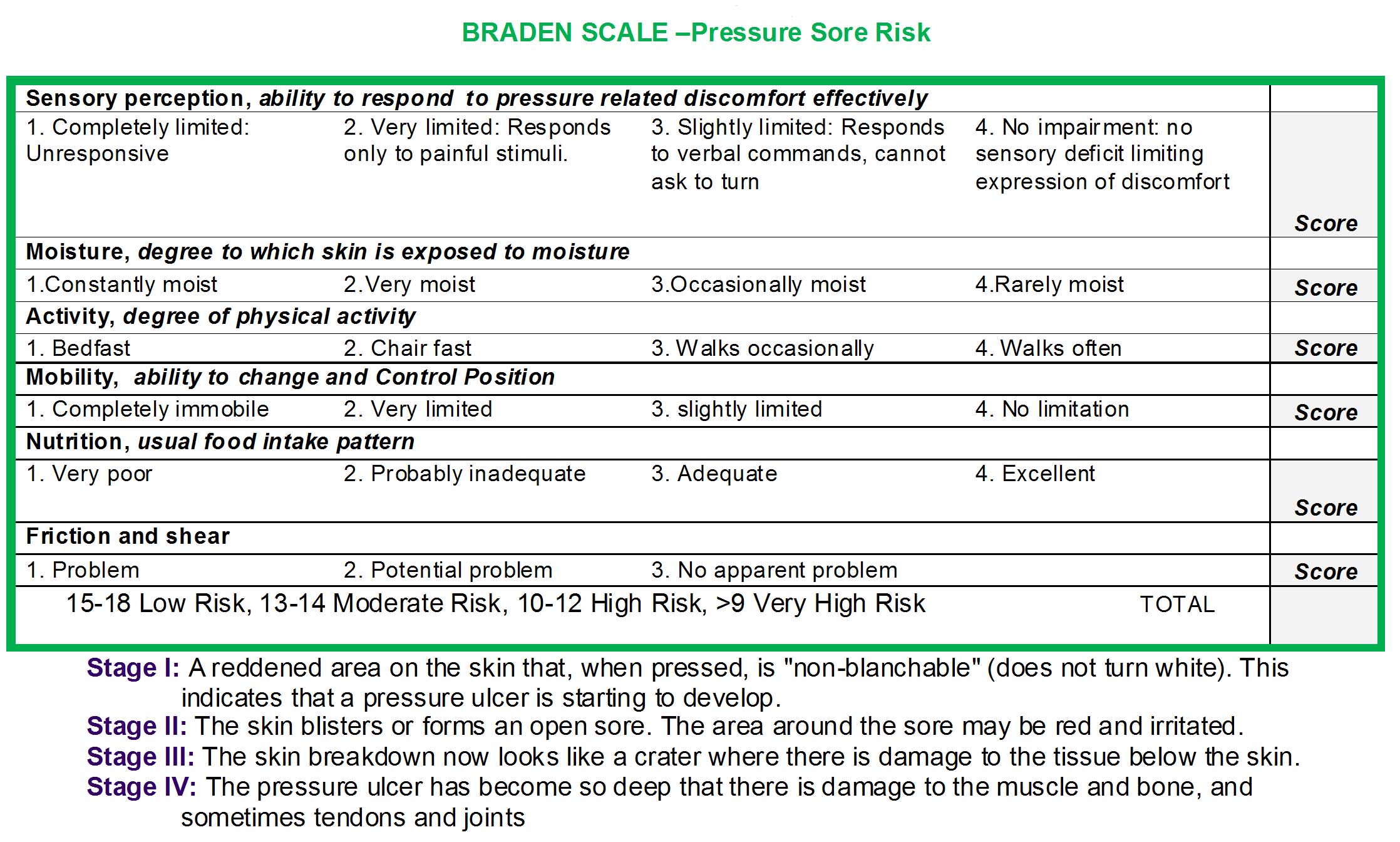
3D: The Braden Scale for Predicting Pressure Sore Risk
Background: This tool can be used to identify patients at-risk for pressure ulcers. The Braden Scale was developed by Barbara Braden and Nancy Bergstrom in 1988 and has since been used widely in the general adult patient population. The scale consists of six subscales and the total scores range from 6-23. A lower Braden score indicates higher levels of risk for pressure ulcer development. Generally, a score of 18 or less indicates at-risk status.
Reference: http://www.bradenscale.com/images/bradenscale.pdf. Reprinted with permission. Hoi4 how to release puppet.
Instructions: Complete the form by scoring each item from 1-4 (1 for low level of functioning and 4 for highest level of functioning) for the first five risk factors and 1-3 for the last risk factor.
Use: Use this tool in conjunction with clinical assessment to determine if a patient is at risk for developing pressure ulcers and plan the care accordingly. In addition to the overall score, abnormal scores on any of the subscales should be addressed in the care plan.
Braden Pressure Ulcer Risk Assessment
Patient's Name ______________________ Evaluator's Name _____________________ Date of Assessment
| Sensory Perception ability to respond meaningfully to pressure-related discomfort | 1. Completely Limited: Unresponsive (does not moan, flinch, or grasp) to painful stimuli, due to diminished level of consciousness or sedation. OR limited ability to feel pain over most of body surface. | 2. Very Limited: Responds only to painful stimuli. Cannot communicate discomfort except by moaning or restlessness. OR has a sensory impairment which limits the ability to feel pain or discomfort over 1/2 of body. | 3. Slightly Limited: Responds to verbal commands, but cannot always communicate discomfort or need to be turned. OR has some sensory impairment which limits ability to feel pain or discomfort in 1 or 2 extremities. | 4. No Impairment: Responds to verbal commands, has no sensory deficit which would limit ability to feel or voice pain or discomfort. |
| Moisture degree to which skin is exposed to moisture | 1. Constantly Moist: Skin is kept moist almost constantly by perspiration, urine, etc. Dampness is detected every time patient is moved or turned. | 2. Very Moist: Skin is often, but not always, moist. Linen must be changed at least once a shift. | 3. Occasionally Moist: Skin is occasionally moist, requiring an extra linen change approximately once a day. | 4. Rarely Moist: Skin is usually dry, linen only requires changing at routine intervals. |
| Activity degree of physical activity | 1. Bedfast: Confined to bed. | 2. Chairfast: Ability to walk severely limited or non-existent. Cannot bear weight and/or must be assisted into chair or wheelchair. | 3. Walks Occasionally: Walks occasionally during day, but for very short distances, with or without assistance. Spends majority of each shift in bed or chair. | 4. Walks Frequently: Walks outside the room at least twice a day and inside room at least once every 2 hours during waking hours. |
| Mobility ability to change and control body position | 1. Completely Immobile: Does not make even slight changes in body or extremity position without assistance. | 2. Very Limited: Makes occasional slight changes in body or extremity position but unable to make frequent or significant changes independently. | 3. Slightly Limited: Makes frequent though slight changes in body or extremity position independently. | 4. No Limitations: Makes major and frequent changes in position without assistance. |
| Nutrition usual food intake pattern | 1. Very Poor: Never eats a complete meal. Rarely eats more than 1/3 of any food offered. Eats 2 servings or less of protein (meat or dairy products) per day. Takes fluids poorly. Does not take a liquid dietary supplement. OR is NPO and/or maintained on clear liquids or IV's for more than 5 days. | 2. Probably Inadequate: Rarely eats a complete meal and generally eats only about 1/2 of any food offered. Protein intake includes only 3 servings of meat or dairy products per day. Occasionally will take a dietary supplement. OR receives less than optimum amount of liquid diet or tube feeding. | 3. Adequate: Eats over half of most meals. Eats a total of 4 servings of protein (meat, dairy products) each day. Occasionally will refuse a meal, but will usually take a supplement if offered. OR is on a tube feeding or TPN regimen which probably meets most of nutritional needs. | 4. Excellent: Eats most of every meal. Never refuses a meal. Usually eats a total of 4 or more servings of meat and dairy products. Occasionally eats between meals. Does not require supplementation. |
| Friction and Shear | 1. Problem: Requires moderate to maximum assistance in moving. Complete lifting without sliding against sheets is impossible. Frequently slides down in bed or chair, requiring frequent repositioning with maximum assistance. Spasticity, contractures or agitation lead to almost constant friction. | 2. Potential Problem: Moves feebly or requires minimum assistance. During a move skin probably slides to some extent against sheets, chair, restraints, or other devices. Maintains relatively good position in chair or bed most of the time but occasionally slides down. | 3. No Apparent Problem: Moves in bed and in chair independently and has sufficient muscle strength to lift up completely during move. Maintains good position in bed or chair at all times. |
3E: Norton Scale
Background: This tool can be used to identify patients at-risk for pressure ulcers. The Norton Scale was developed in the 1960s and is widely used to assess the risk for pressure ulcer in adult patients. The five subscale scores of the Norton Scale are added together for a total score that ranges from 5-20. A lower Norton score indicates higher levels of risk for pressure ulcer development. Generally, a score of 14 or less indicates at-risk status.
Reference: Norton D, McLaren R, Exton-Smith AN. An investigation of geriatric nursing problems in the hospital. London, UK: National Corporation for the Care of Old People (now the Centre for Policy on Ageing); 1962. Reprinted with permission.
Instructions: Complete the form by scoring each item from 1-4. Put 1 for low level of functioning and 4 for highest level functioning.
Use: Use this tool in conjunction with clinical assessment to determine if a patient is at risk for developing pressure ulcers.
| Physical condition | Mental condition | Activity | Mobility | Incontinent | Total Score | ||||
|---|---|---|---|---|---|---|---|---|---|
| Good | 4 | Alert | 4 | Ambulant | 4 | Full | 4 | Not | 4 |
| Fair | 3 | Apathetic | 3 | Walk-help | 3 | Slightly limited | 3 | Occasional | 3 |
| Poor | 2 | Confused | 2 | Chair-bound | 2 | Very limited | 2 | Usually-Urine | 2 |
| Very bad | 1 | Stupor | 1 | Stupor | 1 | Immobile | 1 | Doubly | 1 |
3F: Care Plan
Background: Developing a care plan specific to the needs of each individual patient is critical. This tool is a sample care plan that gives specific examples of actions that should be performed to address a patient's needs. This example is based on the pressure ulcer risk assessment captured with the Braden Scale.
Reference: Developed by Zulkowski, Ayello, and Berlowitz (2010). Used with permission.
Instructions: This tool includes examples of interventions that may be considered for specific scores on each Braden subscale, along with the nurse and Certified Nursing Assistant (CNA) responsibilities for care provision. These should be tailored to meet the needs of your patient and used as examples of how all levels of unit staff have responsibilities for pressure ulcer prevention.
Use: Individualize the care plan to address the needs of at-risk patients.
Sample Care Plan
| Braden Category | Braden Score: 1 | Braden Score: 2 | Braden Score: 3 | Braden Score: 4 |
|---|---|---|---|---|
| Sensory Perception | Completely limited
| Very limited
| Slightly limited
| No limitation
|
| Moisture | Constantly Moist
| Moist
| Occasionally Moist
| Rarely Moist
|
| Activity | Bedfast
| Chairfast
| Walks Occasionally
| Walks Frequently
|
| Mobility | Completely Immobile
| Very Limited
| Slightly Limited
| No Limitations
|
| Nutrition | Very Poor
| Probably Inadequate
| Adequate
| Excellent
|
| Friction and Shear | Problem
| Potential Problem
| No apparent problem
|
3G: Patient and Family Education Booklet
Background: This is an example of an education booklet that can be handed out to patients at-risk for pressure ulcers and their families. The booklet was developed by the New Jersey Collaborative to Reduce the Incidence of Pressure Ulcers.
Reference: Available at: http://www.njha.com/qualityinstitute/pdf/pubrochure.pdf.
4A: Assigning Responsibilities for Using Best Practice Bundle
Background: This tool can be used to determine who will be responsible for each of the tasks identified in your bundle of best practices for preventing pressure ulcers. One way to generate interest and buy-in from the staff is to ask them to self-assign their responsibilities from a prioritized list of tasks that need to be accomplished.
Reference:Dcr files. Developed by Boston University Research Team. Winzip 6 2 – mac edition of established compression utility.
Instructions: Complete the table by entering the different best practices and the specific individuals who will be responsible for completing each task.
Use: Use this tool to assign and clarify the roles and responsibilities of each staff member.
| What practices will we use? | Who will be responsible? |
|---|---|
| Example: Perform comprehensive skin assessment on admission, daily or if condition deteriorates. | Example: RN |
4B: Staff Roles
Background: Delivery 32202. This table gives an example of how responsibilities may be assigned among different staff members.
Reference: Developed by Boston University Research Team.
| Wound care team* | |
|---|---|
| Wound Care Physician |
|
| Certified Wound Care Nurse |
|
| Unit based team | |
| RN |
|
| LPN |
|
| CNA |
|
| Hospitalist |
|
| Other staff, such as dietitian, physical therapist, pharmacist, assigned to specific unit |
|
* May be large or small group that includes nurses and/or physicians in an outpatient or inpatient setting.
4C: Assessing Staff Education and Training
Printable Braden Scale
Background: The purpose of this tool is to assess current staff education practices and to facilitate the integration of new knowledge on pressure ulcer prevention into existing or new practices.
Reference: Adapted from Facility Assessment Checklist developed by Quality Partners of Rhode Island. Available in the Nursing Home section of the MedQIC Web site: https://www.qualitynet.org/dcs/ContentServer?cid=1098482996140&pagename=Medqic%2FMQTools%2FToolTemplate&c=MQTools.
Instructions: Complete the form by checking the response that best describes your facility.
Use: Identify areas for improvement and develop educational programs where they are missing.
Facility Assessment
Date:
A. Does your facility have initial and ongoing education on pressure ulcer prevention and management for both nursing and nonnursing staff?
__ No. If no, this is an area for improvement.
__ This is an area we are working on.
__ Yes.
B. Does your facility's education program for pressure ulcer prevention and management include the following components?
C. What areas of knowledge does the assessment of staff suggest need more attention in education?
| Yes | No | Person Responsible: | Comments: |
|---|---|---|---|
| 1. Are new staff assessed for their need for education on pressure ulcer prevention and management? | |||
| 2. Are current staff provided with ongoing education on the principles of pressure ulcer prevention and management? | |||
| 3. Does education of staff provide discipline-specific education for pressure ulcer prevention and management? | |||
| 4. Is there a designated clinical expert available at the facility to answer questions from all staff about pressure ulcer prevention and management? | |||
| 5. Is the education provided at the appropriate level for the learner (e.g., CNA vs. RN?) | |||
| 6. Does the education provided address risk assessment tools and procedures? | |||
| 7. Does the education include staff training on documentation methods related to pressure ulcers (e.g., location, stage, size, depth, appearance, exudates, current treatment, effect on activities of daily living, pressure redistributing devices used, nutritional support)? |
Functional Status Score for the Intensive Care Unit
Printable Braden Scale Assessment
The Functional Status Score for the Intensive Care Unit (FSS-ICU) is used to evaluate a patient’s physical functioning in an ICU setting. If you wish to access and use the FSS-ICU, please follow this link (to find FSS-ICU, search under the “Physical Outcomes – Tests” heading), and register at this website. Additional resources are available for the FSS-ICU including a pocket card, FAQ, pre-ICU baseline retrospective data collection version, and translated versions. To get updates on revisions to the FSS-ICU and its User Instructions, sign up for the “Newsletter” feature at this website.
Link to FSS-ICU (under “Physical Outcomes – Tests”)
Validation studies of the FSS-ICU
Huang M, et al.Functional Status Score for the ICU: An International Clinimetric Analysis of Validity, Responsiveness, and Minimal Important Difference. Crit Care Med. 2016 Dec;44(12)
Ragavan VK, et al.The Functional Status Score for the Intensive Care Unit Scale: Is It Reliable in the Intensive Care Unit? Can It Be Used to Determine Discharge Placement? JACPT 2016 Aug; 93-100 Link to Article
Johns Hopkins Highest Level of Mobility scale
The Johns Hopkins Highest Level of Mobility (JH-HLM) scale is created to standardize the measurement and reporting of patient mobility in the hospital. The JH-HLM is currently being validated. Anyone wishing to use this scale should submit a user request form.
Survey Of Barriers to Early Mobility
A novel survey instrument to identify important barriers to mobilizing medical inpatients. Results from this paper can assist with the implementation of quality improvement projects for increasing early hospital-based patient mobility.
Manual Muscle Strength Testing
Resistance is applied manually to different muscle groups, and the reviewer grades the strength of the resistance using the Medical Research Council (MRC) scale.
Please click on the picture below to view the Manual Muscle Testing Protocol, published in the Journal of Visualized Experiments.
For more information on surveys instruments and clinical testing methods, please visit: www.ImproveLTO.com.